Research update
In 2018, the Spinal CSF Leak Foundation awarded a research grant to Dr. Kerry Knievel and Dr. Lea Alhilali of the Barrow Neurological Instituted.
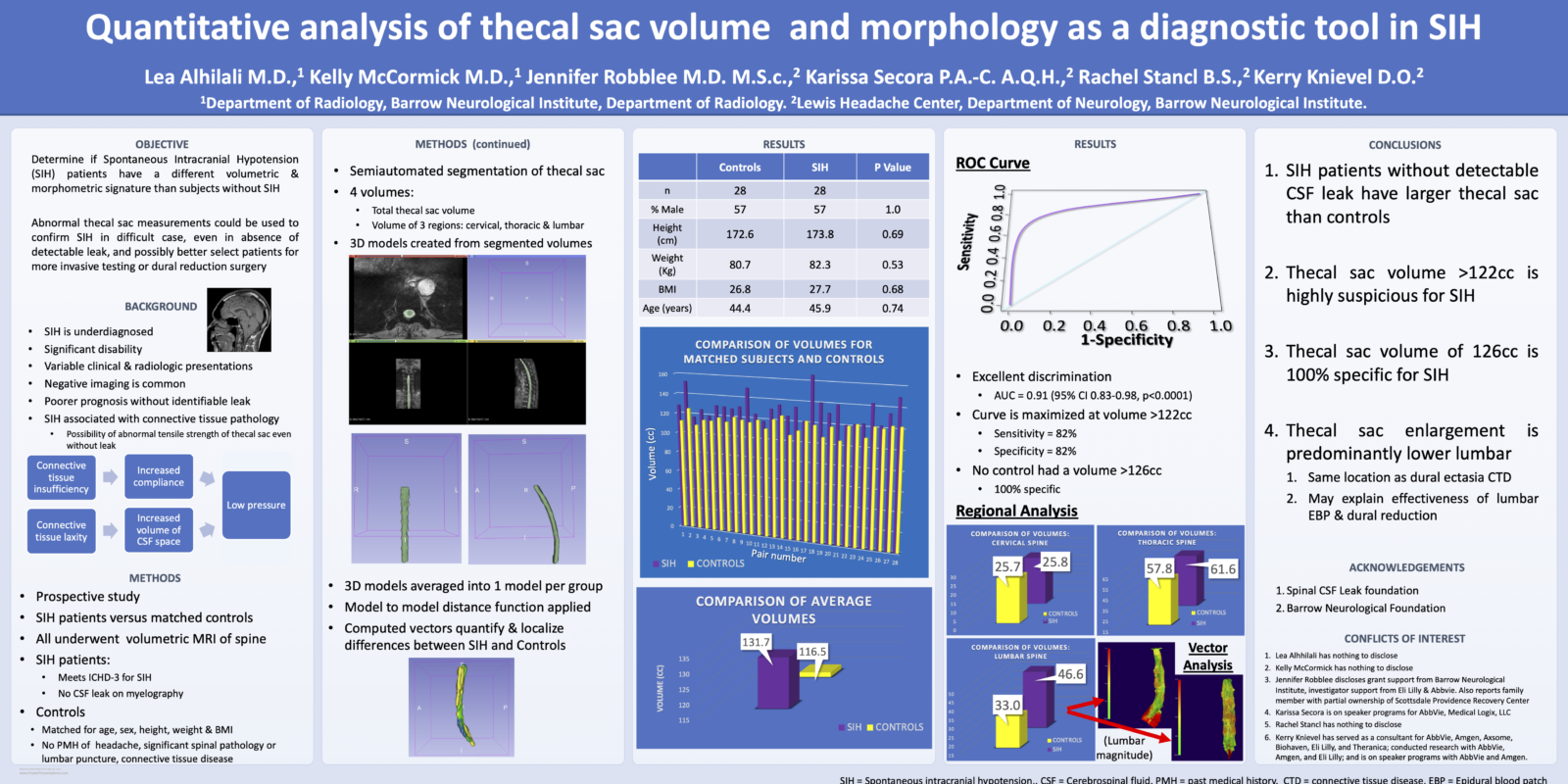
Their study, titled “Quantitative Analysis of Thecal Sac Volume and Morphology as a Diagnostic Tool in SIH,” hypothesized that in some patients, spontaneous intracranial hypotension (SIH) “may result more from an increase in the size of the CSF space or increased compliance from connective tissue insufficiency, rather than from significant changes in CSF volume. Detecting these changes in thecal sac volume and compliance in SIH patients could aid in diagnosis in the significant number of patients in which myelography fails to detect a leak, as well as advance our understanding of the underlying pathophysiology.”
The study sought to determine whether or not “differences in thecal sac volume and quantitative shape features (sphericity, convexity, compactness) are sensitive and specific indicators of SIH in patients without detectable leak, improving diagnosis and treatment in this critical SIH population.”
Promising results
Dr. Knievel and her colleagues presented their early results, including an abstract, paper, and poster, at the American Headache Society’s annual meeting in June. Here is their abstract:
TITLE: Quantitative analysis of thecal sac volume and morphology as a diagnostic tool in SIH
SUMMARY: Quantitative volumetric analysis of the thecal sac can detect enlargement of the thecal sac in spontaneous intracranial hypotension (SIH) patients that may aid in diagnosis of this disorder.
BACKGROUND: The exact mechanism underlying spontaneous intracranial hypotension (SIH) remains unclear; however, the importance of underlying connective tissue pathology has been established in both clinical and laboratory studies. Given the association with connective tissue abnormalities, SIH may result in increased thecal sac size or thecal sac compliance from connective tissue insufficiency. As a result, the thecal sac of SIH patients may have a different volumetric and morphometric signature than subjects without SIH symptoms. The purpose of this study was to develop a new diagnostic tool based on the thecal sac volumetric and morphometric signatures of SIH from quantitative volume and shape analysis.
METHODS: SIH patients and age, gender, and BMI matched controls were prospectively recruited from December 1, 2020 to March 1, 2022. All subjects underwent volumetric MR imaging of the entire spine A semi automated segmentation method was used to extract 3D volumetric models of thecal sac for each subject. Comparison of total thecal sac volume as well as regional volumes were compared between subjects and controls with a paired t-test. Thecal sac models for controls and patients were then averaged among each cohort to create a single average model for each group from the labelmap representations. Subsequently, a signed model to model distance function was used to compute and visualize the correspondent vectors that quantify the localized differences between the models of the average thecal sac for controls and SIH patients. These vectors quantify the differences in shape along the thecal sac anatomy between the two groups.
RESULTS: 28 SIH patients (mean age 45.9 years, mean BMI 27.7, 57% male) and 28 controls (mean age 44.4 years, mean BMI 26.8, 57% male) were recruited. There was no significant difference between the groups in terms of gender (p=1.0), height (p=0.69), weight (p=0.53), BMI (p=0.68), or age (p=0.74). The thecal sac was significantly larger in SIH patients (mean 131.7 cc, 95%CI 108.1-155.3) than in controls (mean 116.5 cc, 95%CI 105.1-127.9, p<0.0001). Thecal sac volume had excellent discrimination for detecting SIH (AUC=0.91, 95%CI 0.83-0.98, p<0.0001). A volume greater than 122 cc was 82% sensitive and 82% specific for SIH, while a volume greater than 126 cc was diagnostic of SIH. Regional analysis demonstrated no significant difference in the cervical thecal sac volume between SIH patients and controls (25.8 and 25.7 cc, respectively, p=0.95), while the thoracic volume was slightly higher in SIH patients than controls (61.6 and 57.8 cc, respectively, p=0.02), and the lumbar volume was notably higher (46.6 and 33.0 cc, respectively, p<0.0001). Model to model distance vector analysis demonstrated that this difference was predominantly in the lower lumbar thecal sac (Figure 1).
CONCLUSION: SIH patients demonstrate a significantly larger thecal sac than controls and the thecal sac volume can be used to effectively diagnose these SIH patients. The enlargement of the thecal sac in SIH patients predominantly occurs in the lower lumbar region, in the same location where dural ectasia occurs in patients with connective tissue disease.
Further reading:
Please see our Research page for more information about the research we fund thanks to your donations.

