Because September is Chiari Awareness Month, we wish to draw attention to a diagnostic pitfall where intracranial hypotension (low intracranial cerebrospinal fluid volume/pressure) due to spinal cerebrospinal fluid (CSF) leak is concerned.
When MRI of the brain is reviewed in patients with intracranial hypotension secondary to spinal CSF leak, there are several findings that may be present in many (but not all) cases. The mnemonic SEEPS coined by Schievink summarizes these findings. [1]
The sagging of the brain is evident through the identification of several features, one of which is descent of the cerebellar tonsils, which may mimic a Chiari type 1 malformation. The cerebellum is the part of the brain that is located at the lower back part of the skull. The cerebellar tonsils are part of the cerebellum. Chiari malformation is congenital and is characterized by descent of the cerebellar tonsils and is often associated with underdevelopment of the posterior cranial fossa (lower back part of skull). In cases of intracranial hypotension with cerebellar tonsillar descent, there is ALSO descent of the midbrain which is absent in congenital Chiari, so the two are distinguishable on MRI. Tonsillar descent in intracranial hypotension has been variably described as acquired Chiari, Chiari mimic, pseudo-Chiari and reversible Chiari but these terms can be confusing. [2–11]
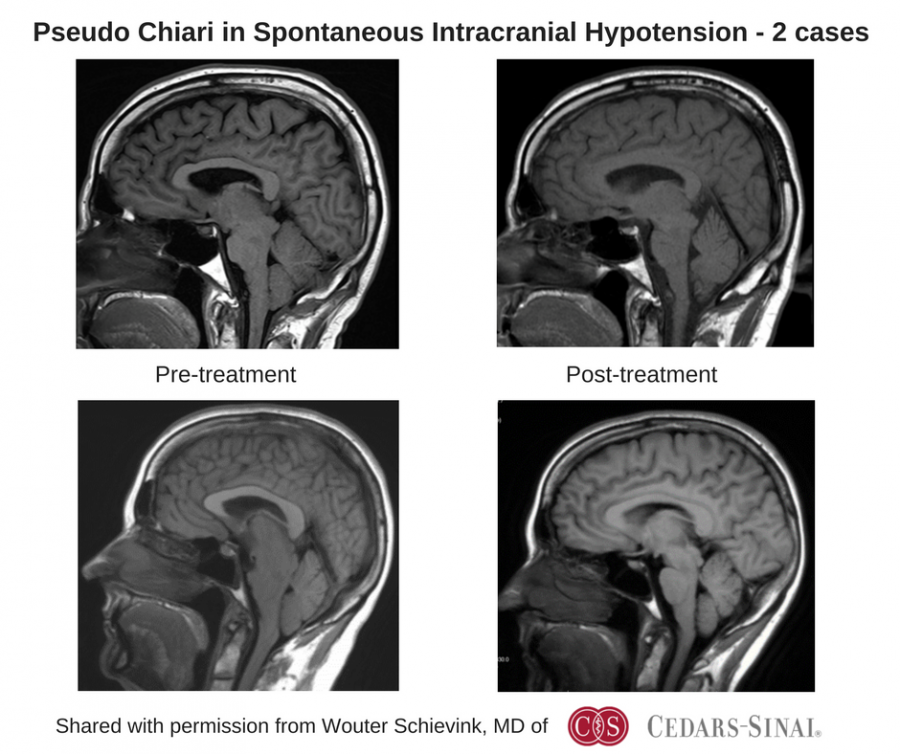
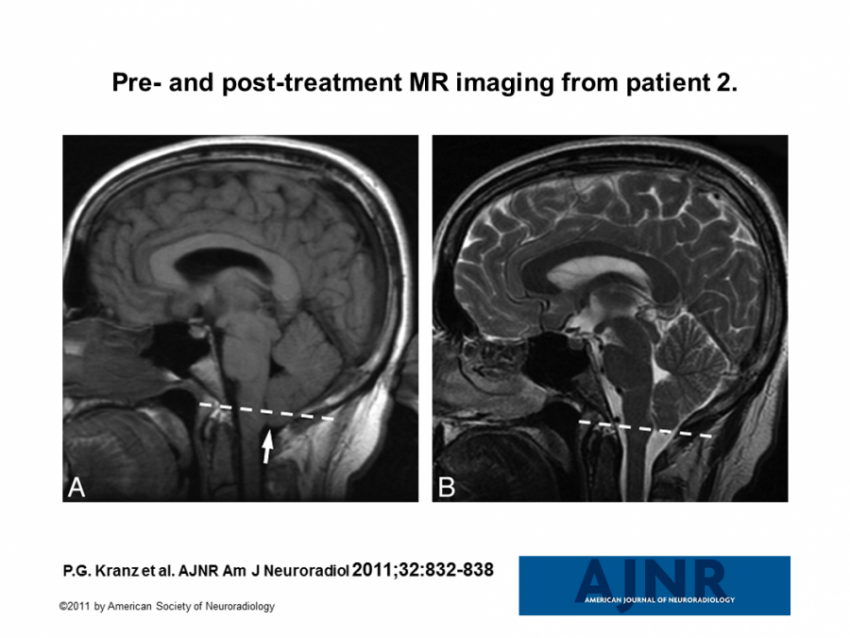
It is evident from published cases that this cerebellar tonsillar descent is reversible in some patients when the intracranial hypotension is successfully treated. [2–4, 12] Examples of such pre-treatment and post-treatment imaging have been provided by Wouter Schievink, MD of Cedars Sinai in Los Angeles, CA and by Peter Kranz, MD of Duke University Medical Center.
The reversibility of the low-lying cerebellar tonsils with treatment of spontaneous intracranial hypotension suggests that the size and shape of the posterior (back) fossa (compartment) of the skull seen in classic congenital Chiari 1 malformation may not be an underlying factor. Milorat and colleagues have studied the mechanism of cerebellar tonsillar herniation in a variety of circumstances and found that not all cases involve a smaller volume of the posterior cranial fossa. [13] Their series published in 2010 included 28 cases associated with intracranial hypotension secondary to lumbo-peritoneal shunting (diversion of CSF from lumbar spine region to peritoneum); these cases with intracranial hypotension had a normal posterior cranial fossa volume.
Complicating the picture is the fact that spontaneous intracranial hypotension is associated with heritable disorders of connective tissue through abnormalities of the spinal dura. [14–16] This subset of patients also has a higher prevalence of Chiari with associated posterior fossa (back compartment of skull) abnormalities. [17, 18] Patients with spontaneous intracranial hypotension may have tonsillar descent related to the intracranial hypotension alone or due to congenitally abnormal posterior cranial fossa exacerbated by intracranial hypotension.
Over the past two decades, patients with cerebellar tonsillar descent have at times been diagnosed erroneously with Chiari type 1 and subsequent Chiari decompression surgery was not helpful. Later the correct diagnosis of spontaneous intracranial hypotension was made and treatment was then appropriately directed. Again, in intracranial hypotension, cranial MRI will show evidence of structures in the middle of the brain to sag and often other SEEPS findings, so in most cases, it can be distinguished from congenital Chiari by radiologists experienced in recognizing these findings. It has been suggested by several authors that when cerebellar tonsillar descent is seen on cranial MRI, that other diagnoses such as spontaneous intracranial hypotension from spinal CSF leak should be ruled out, since therapy should be directed at the underlying cause. [1–4, 6, 12, 13, 19]
References:
1. Schievink WI (2006) Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA 295:2286–2296
2. Atkinson JL, Weinshenker BG, Miller GM, Piepgras DG, Mokri B (1998) Acquired Chiari I malformation secondary to spontaneous spinal cerebrospinal fluid leakage and chronic intracranial hypotension syndrome in seven cases. J Neurosurg 88:237–242
3. Kasner SE, Rosenfeld J, Farber RE (1995) Spontaneous intracranial hypotension: headache with a reversible Arnold-Chiari malformation. Headache 35:557–559
4. Schievink WI (2003) Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol 60:1713–1718
5. Puget S, Kondageski C, Wray A, Boddaert N, Roujeau T, Di Rocco F, Zerah M, Sainte-Rose C (2007) Chiari-like tonsillar herniation associated with intracranial hypotension in Marfan syndrome. Case report. J Neurosurg 106:48–52
6. Mea E, Chiapparini L, Leone M, Franzini A, Messina G, Bussone G (2011) Chronic daily headache in the adults: differential diagnosis between symptomatic Chiari I malformation and spontaneous intracranial hypotension. Neurol Sci 32 Suppl 3:S291–4
7. Samii C, Möbius E, Weber W, Heienbrok HW, Berlit P (1999) Pseudo Chiari type I malformation secondary to cerebrospinal fluid leakage. J Neurol 246:162–164
8. Smith RM, Garza I, Robertson CE (2015) Chronic CSF leak causing syringomyelia and pseudo-Arnold-Chiari malformation. Neurology 85:1994
9. Mokri B (2014) Spontaneous CSF leaks: low CSF volume syndromes. Neurol Clin 32:397–422
10. Wrobel Goldberg S, Young W (2016) Headache rounds: sudden onset chronic daily headache. Headache 56:379–388
11. Holbrook J, Saindane AM (2016) Imaging of Intracranial Pressure Disorders. Neurosurgery. doi: 10.1227/NEU.0000000000001362
12. Kranz PG, Viola RJ, Gray L (2011) Resolution of syringohydromyelia with targeted CT-guided epidural blood patching. J Neurosurg 115:641–644
13. Milhorat TH, Nishikawa M, Kula RW, Dlugacz YD (2010) Mechanisms of cerebellar tonsil herniation in patients with Chiari malformations as guide to clinical management. Acta Neurochir (Wien) 152:1117–1127
14. Schievink WI, Gordon OK, Tourje J (2004) Connective tissue disorders with spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension: a prospective study. Neurosurgery 54:65–70; discussion 70
15. Reinstein E, Pariani M, Bannykh S, Rimoin DL, Schievink WI (2013) Connective tissue spectrum abnormalities associated with spontaneous cerebrospinal fluid leaks: a prospective study. Eur J Hum Genet 21:386–390
16. Mokri B, Maher CO, Sencakova D (2002) Spontaneous CSF leaks: underlying disorder of connective tissue. Neurology 58:814–816
17. Castori M, Morlino S, Ghibellini G, Celletti C, Camerota F, Grammatico P (2015) Connective tissue, Ehlers-Danlos syndrome(s), and head and cervical pain. Am J Med Genet C Semin Med Genet 169C:84–96
18. Martin VT, Neilson D (2014) Joint hypermobility and headache: the glue that binds the two together–part 2. Headache 54:1403–1411
19. Rahman M, Bidari SS, Quisling RG, Friedman WA (2011) Spontaneous intracranial hypotension: dilemmas in diagnosis. Neurosurgery 69:4–14; discussion 14