My Year of Adaptation: What I Learned Putting ADAPT into Action
By Jodi Blaszyk, PsyD
Last year, during mental health awareness month, I shared with the Spinal CSF Leak Foundation community a mental health strategy I coined called ADAPT, for support in living with spinal CSF leak.
Over this past year, I’ve had to use the techniques of ADAPTing more than I ever realized.
The core concepts embedded in the acronym ADAPT are Acceptance, Diagnosis, Advocate and educate, Plan, and Thrive. These aren’t stages that a person experiences linearly, but rather ideas that can help us attend to our mental well-being at any time during the process of living with a spinal CSF leak.
As May’s Mental Health Awareness Month comes to a close, I’d like to reflect and revisit what it has meant to me, personally, to use ADAPT in my life.
Acceptance and Diagnosis
Three years ago, I had what I thought was my last treatment for spinal CSF leak. Though my leak location was never firmly identified, I was patched with fibrin glue. This sent me into unrelenting high pressure for many months. (For more information about rebound intracranial hypertension, you can view the slides of a talk by Dr. Deborah Friedman here.) Gradually, however, the high pressure faded, and by last spring I began to recognize the return of the familiar pain of my old life. My leak was back.
As my symptoms increased, I worked on building up the physical and emotional energy to face the leak pursuit anew. It was hard to feel like I had to start all over, but I tried to accept where I was. I reminded myself that enough time had passed that perhaps my “cold case” could be reopened, and perhaps new imaging could even give me that elusive thing every person with a leak yearns for: a confirmed diagnosis.
But I also knew that I needed to accept the possibility that my leak pursuit might not yield anything new. To help me come to terms with that, I imagined a scenario where my case would not be closed again, but merely shelved until new technology or research could illuminate a new path forward. With a poppy seed of hope, I imagined myself taking back the sense of power I had lost to my leak and reclaiming the old Jodi.
Advocating and educating
Once I decided to begin pursuing treatment for my leak yet again, I felt it was important to protect myself. I found it anchoring to accept that one or two better symptom days usually signaled that a few difficult ones would follow. Understanding that I could count on my leak experience to wax and wane became a kind of solace. And knowing this, I was able to plan to do the most on the days when I felt the best.
Also, as I moved ahead to hopefully find the source of my leak and obtain a lasting treatment, I tried not to get stuck on past appointments that had left me frustrated or angry. For example, not dwelling on the memorable day when a clinician suggested I did not have a leak and should stop pursuing a diagnosis. I knew he was wrong, but I also knew I had a choice: to get angry, or to continue advocating for myself. I had to lean hard into ADAPT to keep going and not feel stuck in that terrible moment.
My persistence in the face of doubt was important, since in at least one instance, it served to educate: A physician who had evaluated me and dismissed the possibility of my having a spinal CSF leak later called me to apologize. He acknowledged that he had not factored in information regarding findings in my case from a different institution when he ruled out that diagnosis.
However, I also learned that it is perfectly okay for the sake of your emotional health to advocate for yourself and ask for a different clinician.
Planning and thriving
The past year was chock-full of planning. In the midst of my escalating leak symptoms last spring, I started a new job. I didn’t share anything about my condition with anyone at work, and even though I was able to work from home, being efficient on tough symptom days was challenging and involved a lot of planning on my part.
Just as tricky to plan were those little moments when I could thrive. Some days, thriving meant finding enjoyment in things I love to do, and other days it was just about keeping up. I tried to take advantage of those moments when my pain was managed and my energy was higher, allowing myself a moment to thrive while working in my garden.

Jodi finding a moment to thrive in her garden
Putting it all together
After I finally began pursuing treatment in earnest, I was delighted to feel heard and supported by the clinician who eventually took my case. Since it had been four years since my last digital subtraction myelogram (DSM), he recommended I have another round of DSM imaging and scheduled one for me. I was bracing myself for what we might find when my DSM appointments had to be rescheduled unexpectedly.
While this was at first challenging to accept, I soon discovered the timing was actually in my favor: my rescheduled DSMs happened to line up with an availability window for the center’s new Photon Counting CT (PCCT).
In this type of imaging technology, the machine emits a beam of X-ray photons, while special photon-counting detectors capture X-ray photons and measure their energy levels as they pass through a person’s body. The machine uses that information to create an image, similar to a traditional CT scanner, but in this case with much higher resolution. In fact, PCCT images are often so much clearer and more finely detailed than other types of imaging, they can reveal things that other types of imaging technology miss.
Having my DSM appointments during the PCCT availability window meant that if anything suspicious appeared on the DSMs, I could be further imaged using this exciting new technology.
I had to travel for this specialized treatment, and during my stay near the hospital, I found myself enjoying the process. Though I was nervous about what the tests might reveal, I was happy to enjoy having meals, reading, and planning my question-peppering for the doctors. I recognized it for what it was: little moments of thriving.
A diagnosis after all
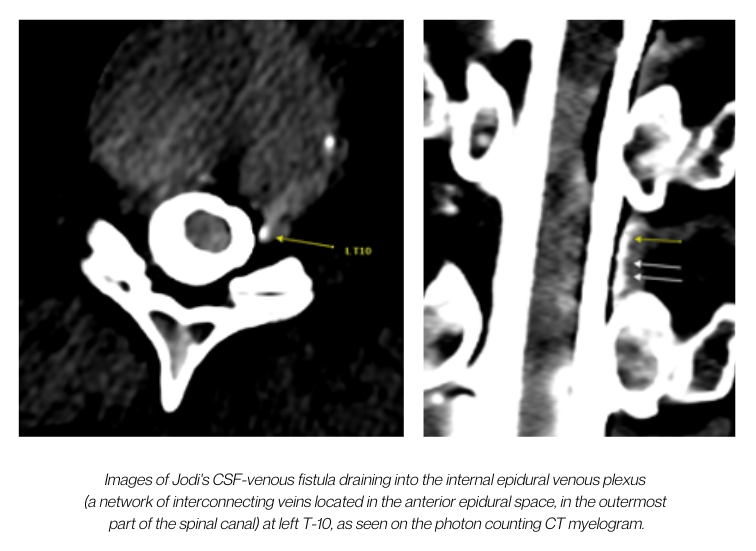
Unlike the last time I had a DSM, this time the tests showed prominent renal contrast and several suspicious areas—undeniable signs of a leak. When I heard the news, I was unable to say anything, I was so shocked. After so long with no answers, it seemed unreal. And then the PCCT revealed what the DSM could only hint at: clear-cut, undeniable proof of my condition, in the form of a CSF-venous fistula.
The fistula was at T-10, on the left side, positioned in a spot so difficult to see on imaging that the doctor told me that not only would the fistula not have been visible without the PCCT, but also that it was only the fifth one his practice had ever seen in that particular location.
Again, I was speechless. I could not have had a more disparate experience from the last time I’d attempted to get to the bottom of my leak. Diagnosis in hand, I went to lunch. I’m sure passersby wondered why the lady sitting alone was smiling.
Adapting to the future
Just the other day, my CSF-venous fistula was treated with embolization. I felt a sense of serendipity, as my procedure day happened to be the five-year anniversary of the very day that I’d lifted a heavy chair and felt a soft pop in my back, unwittingly starting my spinal CSF leak journey.
Today, I am recovering. I’m still journaling, keeping track of my symptoms in case I need notes for later, and taking rare but occasional pain medicine and acetazolamide for my “rebound” top-of-the-head headache. I have started to think about what I would like to do this summer and fall. I know it is possible that I may spring another fistula later. But I may not. My high pressure is not as pronounced as it was last time, and I think I have reason for optimism. I am surely glad I persevered through moments of doubt.
For this year’s Leak Week, I plan to don one of my Spinal CSF Leak Foundation t-shirts and drive to the local family practice. I will drop off a Foundation mug with resource materials rolled up and placed inside. I have been supported by the PA who I see there, and I know that others with a leak will likely pass through her office. I am certain she will advocate for her patients and educate her colleagues.
As for myself, no matter what is in store for me, I will continue to adapt and continue to reflect on the ADAPT principles as I navigate this part of my leak experience. At times I’ve thought that living with a leak was like having a physical and emotional ball and chain. But now, as I look out at the river behind my house, I’m thinking about getting a fishing boat, and how I’ll need not a ball and chain but an anchor.
Further reading:
For more about ADAPT:
Click here to read about the first letter in the ADAPT acronym: Acceptance.
Click here to read about the next letter in the ADAPT acronym: Diagnosis.
Click here to read about the next letter in the ADAPT acronym: Advocate (and educate).
Click here to read about the next letter in the ADAPT acronym: Plan.
Click here to read about the final letter in the ADAPT acronym: Thrive.
This content is provided for general informational and educational purposes only and is not intended or implied to be a substitute for professional medical advice, help, diagnosis, or treatment. If you think you have an emergency, please call your doctor or emergency services immediately. To find a mental health provider, you can visit the ADAA Find a Therapist directory. If you are in a mental health crisis, call the National Suicide Prevention Lifeline at 1-800-273-8255 or reach out to the Crisis Text Line by texting HOME to 741741 to connect with a crisis counselor.


