In recent years, the awareness of spontaneous intracranial hypotension (SIH) has increased such that more patients are being diagnosed correctly. But sadly, misdiagnosis remains the rule rather than the exception. Too many suffer for months, years, or even decades without the correct diagnosis. The often-severe positional headache and other neurological symptoms can be profoundly disabling. Because SIH has an identifiable underlying cause, a spinal cerebrospinal (CSF) leak, it is often treatable with the guidance of specialized diagnostic testing as needed. Each prompt and correct diagnosis of SIH increases the chance of a durable cure. We examine the common and not-so-common misdiagnoses here to support the reduction of diagnostic errors and delays.
First, see a few comments from physician attendees at the Third Annual Intracranial Hypotension Symposium about common misdiagnoses.
SIH and Common Misdiagnoses
SIH is listed as a secondary headache disorder. Secondary means that there is an underlying cause, in this case, a spontaneous CSF leak at the level of the spine. While orthostatic head pain, or “upright headache,” is the most common manifestation, the range of neurologic symptoms, complications, and severity is broad. The estimated incidence is based on a single urban emergency department study roughly estimating the annual incidence at 5 per 100,000. While this meets the criteria for a rare disease in the USA, this annual incidence estimate is probably an underestimate. More accurate estimates are needed. We do know that SIH isn’t nearly as common as most other causes of headache, which contributes to low awareness, misdiagnosis, and delayed diagnosis.
Migraine
Migraine is a neurological disorder categorized as a primary headache disorder, meaning that it does not have a different underlying cause. It is very common: about 1 in 5 women, 1 in 10 men suffer with migraine. The chronic form occurs in about 2% of the population. The annual prevalence has been reported to be 2.2 %. When health professionals see patients with disabling daily headache, it isn’t surprising that migraine is often considered first. Migraine is the most common misdiagnosis among patients with SIH. An important hallmark of SIH is that migraine treatments are almost entirely ineffective. This is a common theme in many of the patient stories we have shared. See patient stories.
New Daily Persistent Headache
Another common misdiagnosis is “new daily persistent headache” (NDPH). Most patients with SIH can tell you the date that their symptoms began and never left. But “new daily persistent headache” is a diagnosis of exclusion, meaning that underlying and potentially reversible causes have been systematically ruled out. NDPH is usually treated with medications, which, like treatments for migraine, are almost entirely ineffective for SIH.
Cervicogenic Headache
Cervicogenic headache is a headache that arises from problems in the neck. It often manifests with both head pain and neck pain, which are common in SIH patients also, so it is easy to see why this misdiagnosis is so common. Cervicogenic headache can also be worse with upright posture, similar to SIH. Physical therapy often makes SIH symptoms worse due to mobilization of the neck and spine.
Post-Concussion Headache
SIH may onset after a blow to the head or a minor fall. Such a headache is easily labeled as a post-concussion or post-traumatic headache, particularly if imaging was limited to a head CT, or brain MRI was interpreted as normal, and the positional exacerbation was overlooked.
A CT of the head may show some evidence of SIH but is often negative. Brain MRI with gadolinium enhancement is the standard-of-care initial diagnostic imaging for ALL patients suspected of having SIH. About 80-85% of cases will have evidence of SIH on this imaging, but conversely, normal imaging does not rule it out. The SEEPS mnemonic lists the core findings on enhanced brain MRI:
Subdural fluid collections
Enhancement of pachymeninges
Engorgement of venous structures
Pituitary hyperemia
Sagging of the brain (including but not limited to low-lying cerebellar tonsils)
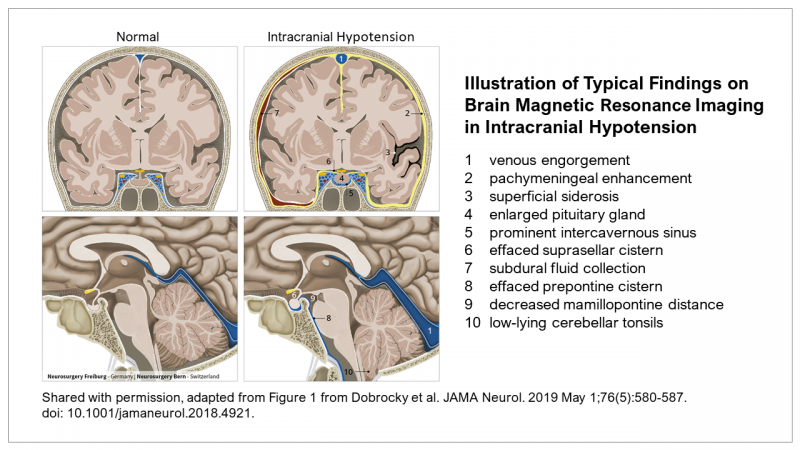
Chiari I Malformation
Because evidence of low-lying cerebellar tonsils is often seen on brain MRI in SIH, it can be confused with Chiari I. For experienced radiologists, neurosurgeons, and neurologists, SIH and Chiari I are easily distinguished.
Pituitary Tumor
The finding of an enlarged pituitary gland can be interpreted as a pituitary tumor leading to a pituitary biopsy. Emily escaped pituitary biopsy, fortunately. See her story.
Subdural Hematoma
Subdural fluid collections and subdural hematomas are seen in about one-third of SIH cases. Subdural hematomas are not always recognized as being secondary to SIH. It is important that treatment of the underlying spinal CSF leak is not overlooked. Lori’s subdural hematomas were literally ignored by her neurologist until she insisted on follow-up imaging. A neurosurgeon then called her to arrange an emergent surgical evacuation of the blood pressing on her brain. Her condition worsened and the SIH diagnosis was still missed for years. See Lori’s story.
Meningitis
In emergency departments, where patients often present with new head pain, often with neck pain or stiffness, another commonly considered diagnosis is meningitis. A lumbar puncture may be performed as part of initial testing. Occasionally, the positional headache is later attributed to a spinal CSF leak due to the lumbar puncture, overlooking that the onset of the symptoms came BEFORE the procedure.
POTS
The poor tolerance of upright posture associated with postural orthostatic tachycardia syndrome (POTS) can mimic intracranial hypotension, but the two may also coexist.
Occipital Neuralgia
The headache in SIH is most often located in the occipital region, or back of the head. This can lead to a misdiagnosis of occipital neuralgia, or pain arising from the occipital nerve.
Trigeminal Neuralgia
Because SIH patients may also experience pain in the distribution of the trigeminal nerve, trigeminal neuralgia may be diagnosed without the recognition of the underlying cause of the pain.
Other Headache
Tension headache and sinus headache are included among other misdiagnoses.
Other Presentations
There are several clinical and/or radiologic presentations and complications that may not be recognized as being secondary to SIH:
- tremor and abnormal gait can be confused with Parkinson’s disease
- cognitive dysfunction in SIH ranges from mild to severe and can be misdiagnosed as a form of dementia
- anxiety and depressive symptoms are common in SIH: headache and neurological symptoms are often attributed to anxiety or depression
- stupor or coma
- cerebral venous thrombosis (venous blood clots in brain)
- ischemic stroke
- non-aneurysmal subarachnoid hemorrhage (brain bleed)
- cerebellar hemorrhage (bleeding in cerebellum)
- reversible cerebral vasoconstriction (syndrome of sudden constriction of arteries in brain)
- posterior reversible encephalopathy syndrome (serious brain swelling syndrome)
- spinal cord herniation
- myelopathy (spinal cord injury or compression)
- bibrachial amyotrophy (arm weakness due to stretching of the nerves in upper spine; mimics ALS)
- quadriplegia (arm and leg weakness)
- syringomyelia (fluid-filled cyst inside spinal cord)
- death
Fictitious disorder
Alarmingly, children and adults alike have been labeled with fictitious disorder (previously called Munchausen Syndrome), which is utterly egregious.
The Future of SIH and Misdiagnosis
Headache neurologists and general neurologists, in particular, are diagnosing SIH more often than just a few years ago, thanks to greater familiarity due to more publications and medical education. There remains a need to elevate awareness among all clinicians.
Learn more about the diagnosis of SIH.
So for Rare Disease Day on February 28 and every day, let’s elevate awareness of SIH, so that more patients can receive the correct diagnosis more quickly, then access appropriate testing and treatment of the underlying cause, spinal CSF leak, for better long-term outcomes. Let’s make misdiagnosis the exception.
.

