Spinal CSF Leak Treatment
Treatment for spinal CSF leak varies from conservative measures to surgical procedures. Some patients have symptoms that resolve spontaneously in a matter of hours, days, or weeks without ever seeking or requiring medical care. However, some serious complications dictate emergent and more aggressive intervention.

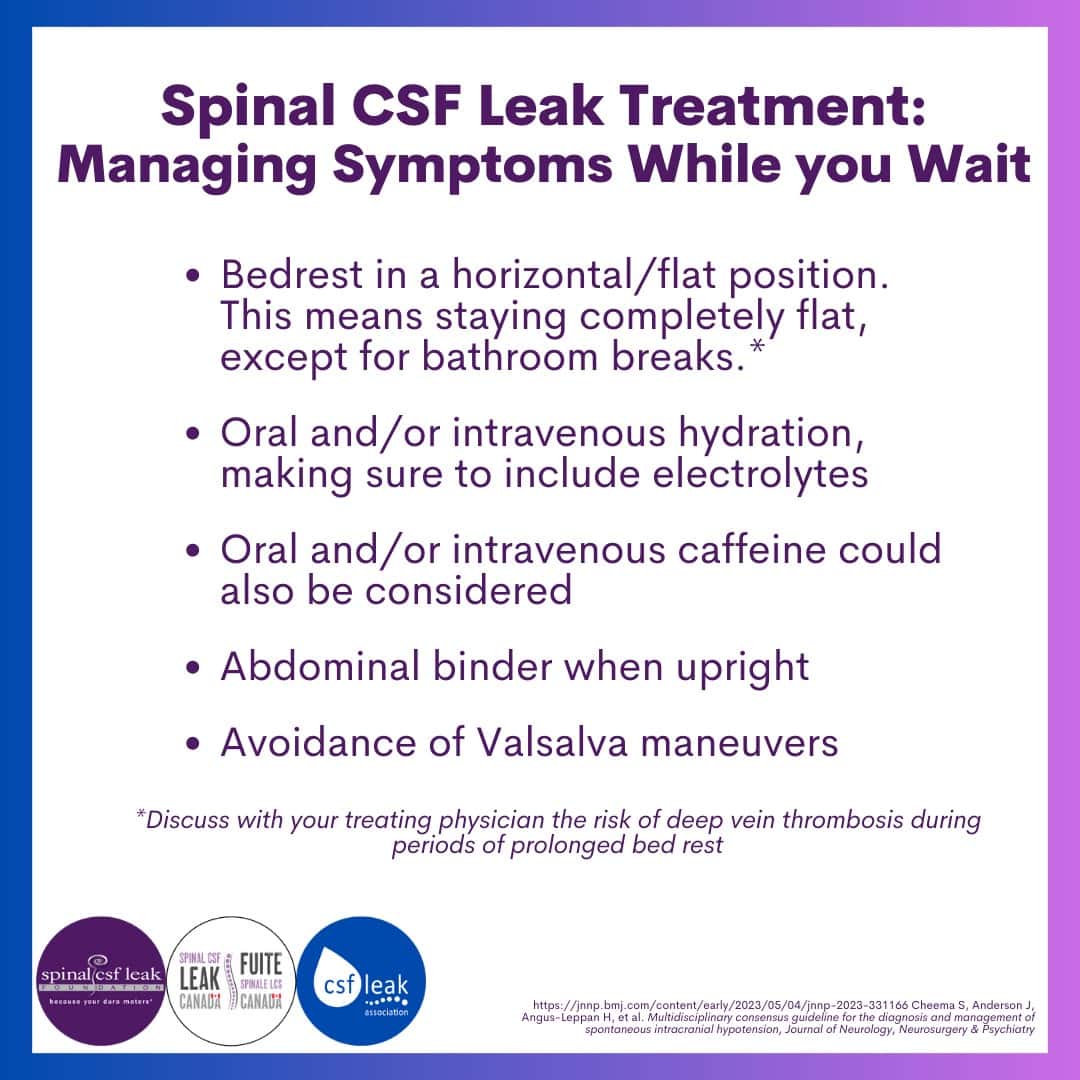
Conservative measures
Conservative measures of managing symptoms while waiting for treatment include complete bedrest (the risk of deep vein thrombosis during periods of prolonged bed rest should be discussed with your treating physician); oral and/or intravenous hydration, including electrolytes; caffeine; wearing an abdominal binder when upright; and avoidance of Valsalva maneuver.
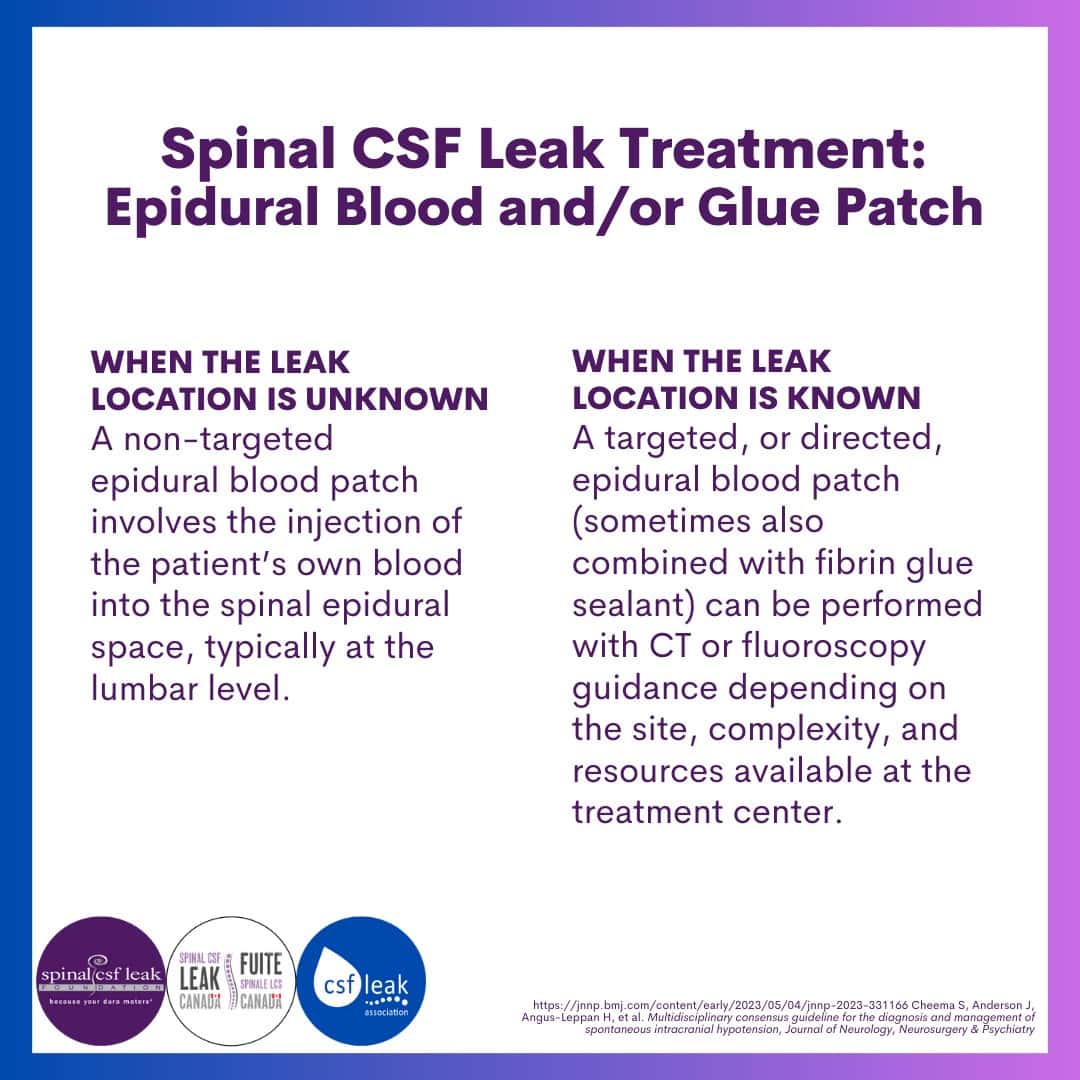
Epidural blood and/or glue patching
In an epidural blood patch (EBP), the patient’s own blood is injected into the epidural space (the space just outside the dura within the spinal canal), forming a “patch” over the dura. An EBP can be targeted (that is, placed at the known location where a patient is leaking, such as a post LP leak) or it can be non-targeted (placed at lumbar or thoracolumbar locations). A non-targeted EBP is usually performed when a leak site has not yet been localized, or for diagnostic purposes. The volume (the amount of the patient’s own blood administered) ranges from small (10 mL) to large (100 mL). When the leak location is known or suspected, epidural patching with fibrin glue sealant may be used.
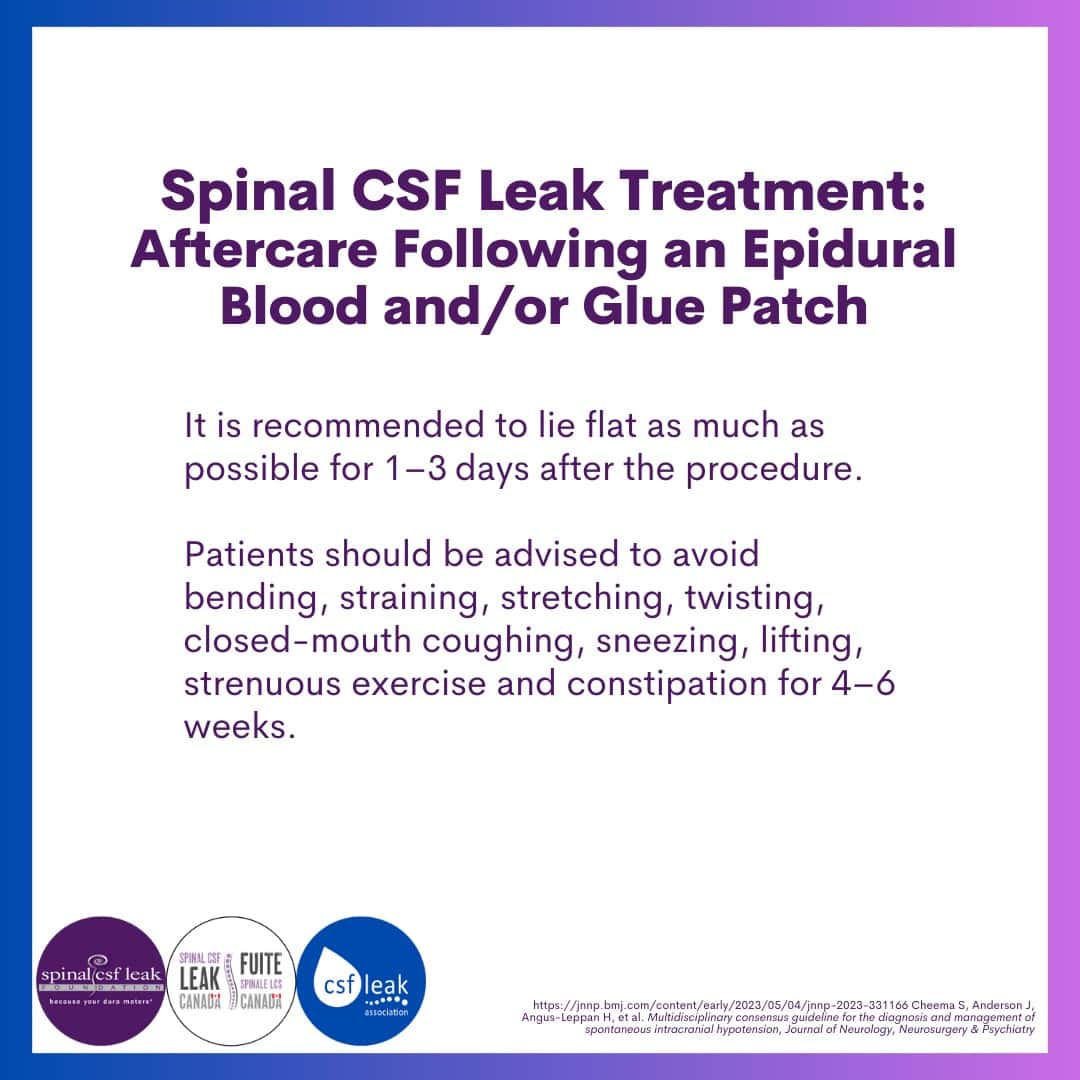
While restrictions after an EBP are individualized, it is typical for physicians to recommend avoidance of bending, lifting, twisting, and straining (valsalva) for about 4-6 weeks.
Surgical treatment
Depending on the nature of the leak, surgical repair may be required. Surgical repairs are often less technically straightforward than might be anticipated, due to frequently noted abnormal dura and the variety of anatomic leak types and locations. The specific approach is tailored to the type and location of the leak and to the individual patient.
In cases where a spinal CSF leak is caused by a CSF-venous fistula, this can be treated by surgery, by glue injection, or by endovascular embolization.

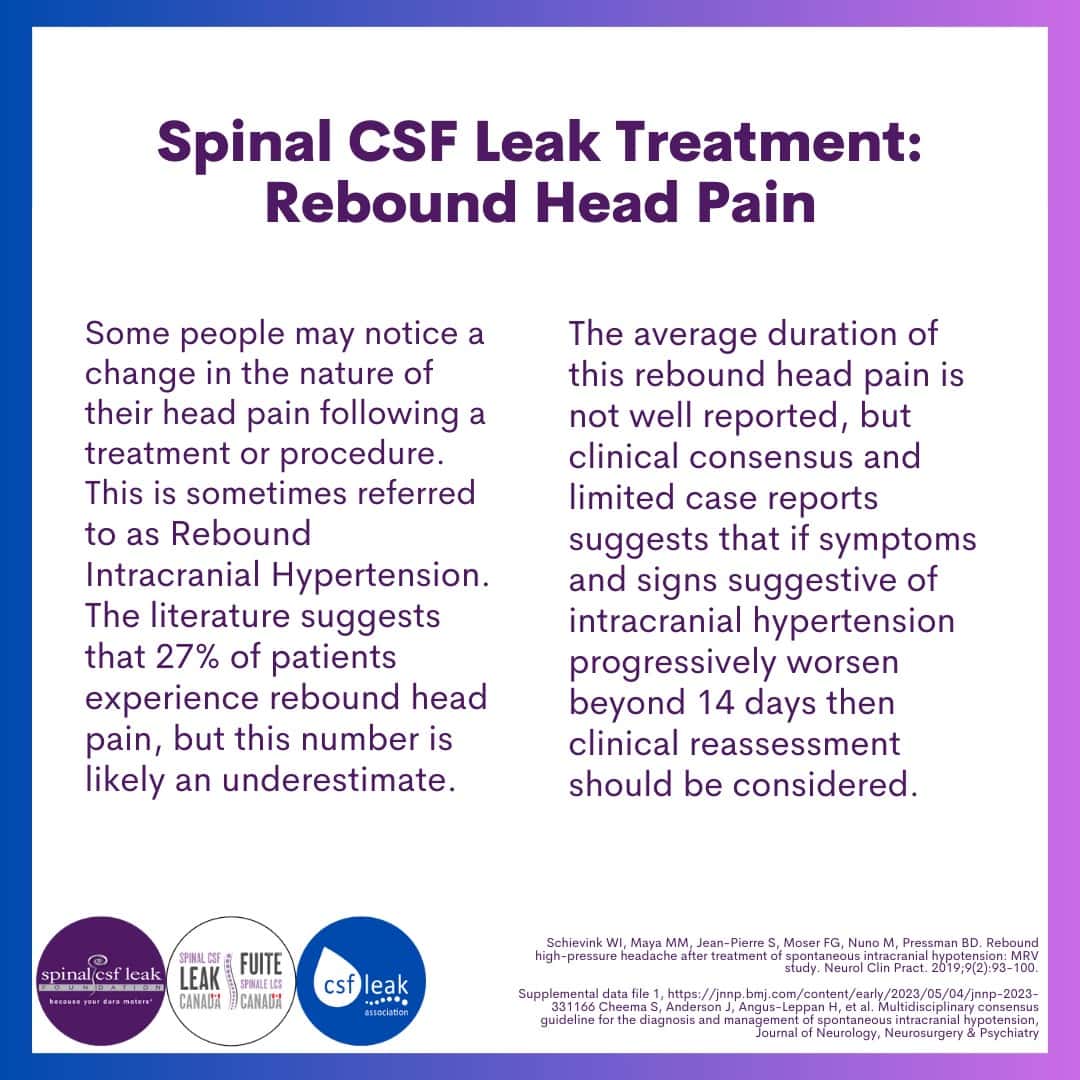
After treatment: Rebound head pain
Following a treatment or surgical procedure, some people may notice a change in the nature of their head pain. This is sometimes referred to as Rebound Intracranial Hypertension. The literature suggests that 27% of patients experience rebound head pain, but this number is likely an underestimate.
The average duration of this rebound head pain is not well reported, but clinical consensus and limited case reports suggests that if symptoms and signs suggestive of intracranial hypertension progressively worsen beyond 14 days then clinical reassessment should be considered.
Another of our medical advisors, Dr. Deborah Friedman, spoke on the subject of RIH and IIH at the 2018 symposium. You can view the slides of her talk here.
Prognosis
References:
Cheema S, Anderson J, Angus-Leppan H, et al. Multidisciplinary consensus guideline for the diagnosis and management of spontaneous intracranial hypotension. Journal of Neurology, Neurosurgery & Psychiatry. Published Online First: 05 May 2023.
Schievink WI, Maya MM, Jean-Pierre S, Moser FG, Nuno M, Pressman BD. Rebound high-pressure headache after treatment of spontaneous intracranial hypotension: MRV study. Neurol Clin Pract. 2019;9(2):93-100.
Coming up tomorrow:
We discuss spinal CSF leak research, and what’s on the horizon.
Further information:
Spinal CSF Leak treatment main page (Spinal CSF Leak Foundation)
