Diagnosis
The word “diagnosis” means “discerning or distinguishing” and comes from an even older Greek word that meant “to know thoroughly” or “know apart from another.” Which is fitting, as one of the most challenging aspects of diagnosing a spinal CSF leak is recognizing it from the presenting symptoms without confusing it for another condition.

The most important clues to the diagnosis of intracranial hypotension lie in the patient history. Gathering information about symptoms and history—including the nature of a patient’s head pain, any recent trauma or medical procedure, any previous diagnoses, known spinal problems, and any pre-existing weakness of connective tissue—is the first step in the diagnostic process.
Diagnostic imaging
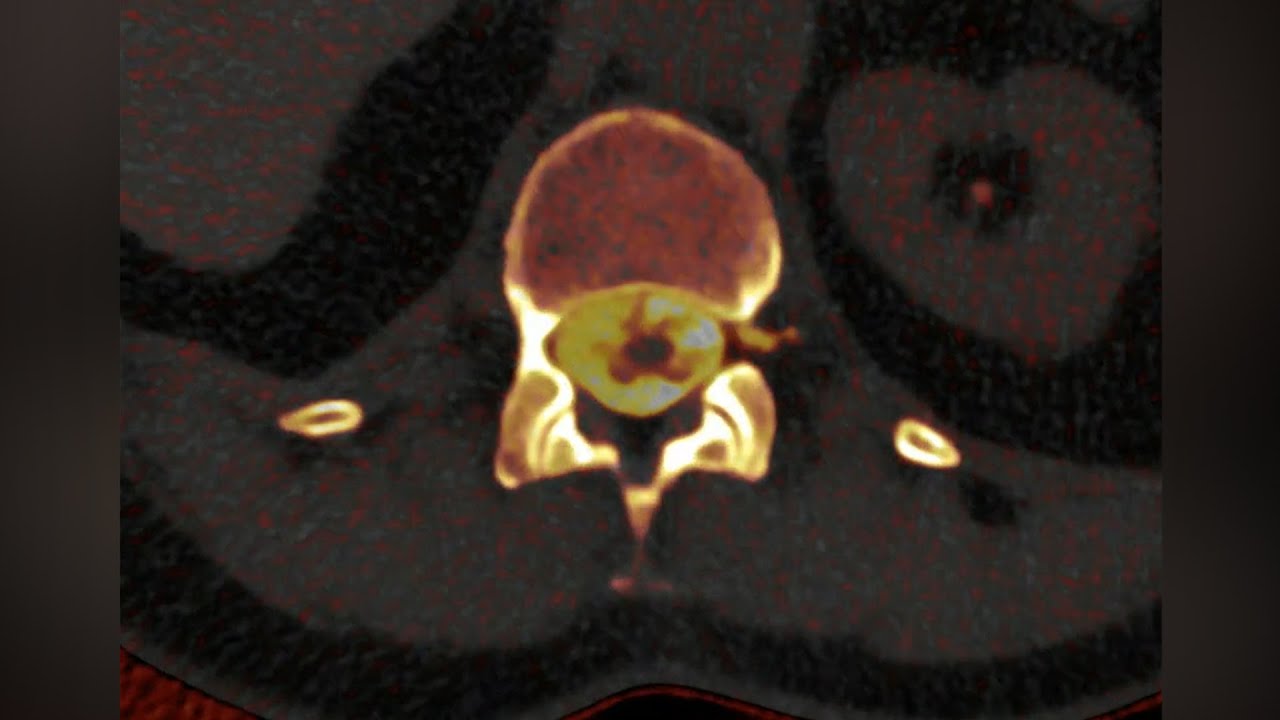
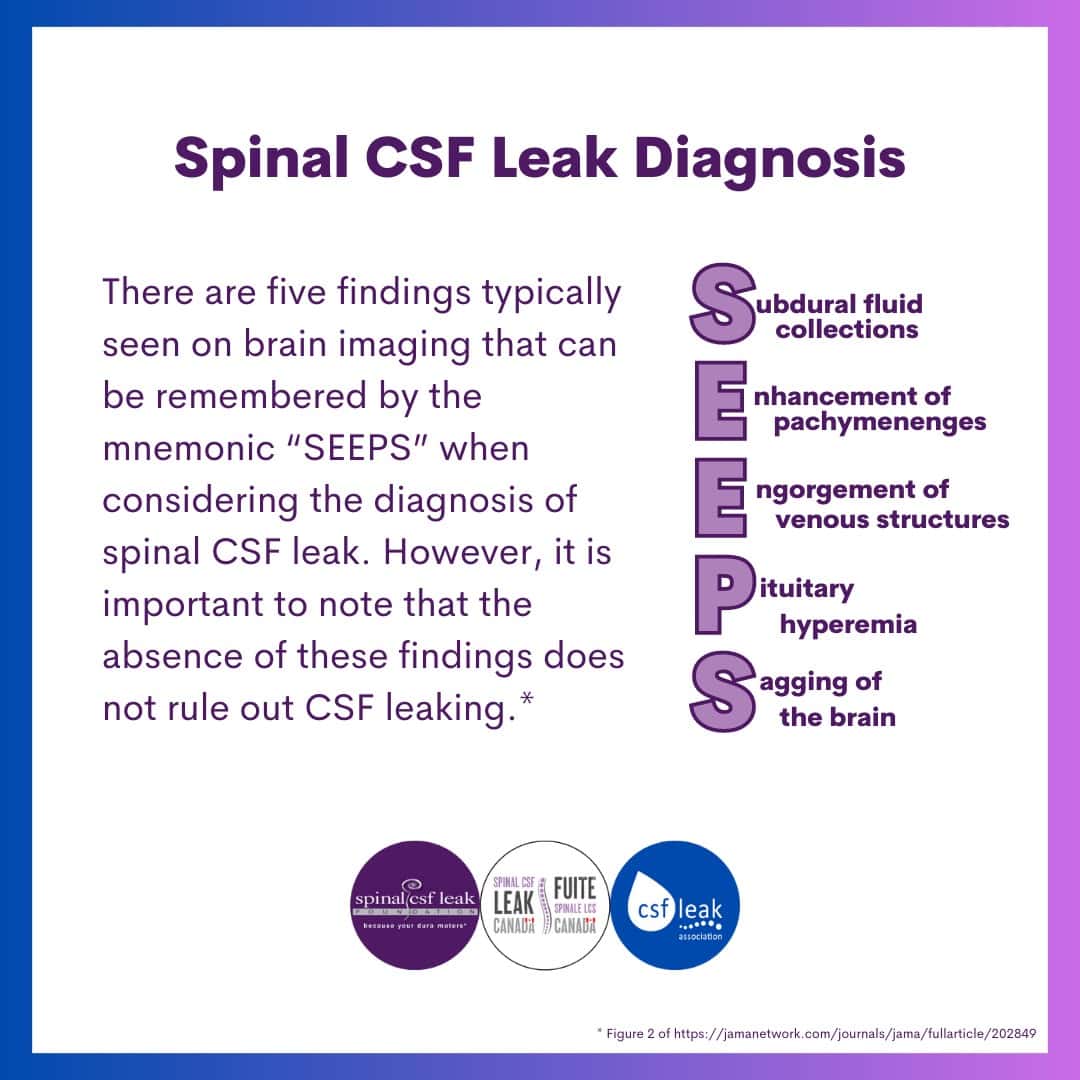
Diagnostic tests for confirming spinal CSF leak can include: MRI of the brain with contrast to look for signs of intracranial hypotension; MRI of the spine to look for possible areas of spinal CSF leak; CT myelogram (injection of radiographic contrast into the spinal canal followed by a CT of the spine to look for leak location); MR myelogram (MR imaging of spine with the use of specific sequencing/weighting); and DSM (digital subtraction myelogram, a myelogram done under fluoroscopy with the additional ability to digitally subtract a pre-contrast image to enhance the visualization of the contrast. This is used to image rapid leaks, ventral leaks, or leaks not associated with an obvious extrathecal CSF collection, such as a CSF-venous fistula.) A lumbar puncture is not required to make the diagnosis.
A new type of imaging technology is the photon counting CT (PCCT). For this kind of imaging, the machine emits a beam of X-ray photons, while special photon-counting detectors capture X-ray photons and measure their energy levels as they pass through a person’s body. The machine then uses that information to create an image, similar to a traditional CT scanner, but in this case with much higher resolution. In fact, PCCT images are often so much more finely detailed than other types of imaging, they can reveal things that other types of imaging technology miss.
The path to diagnosis and treatment
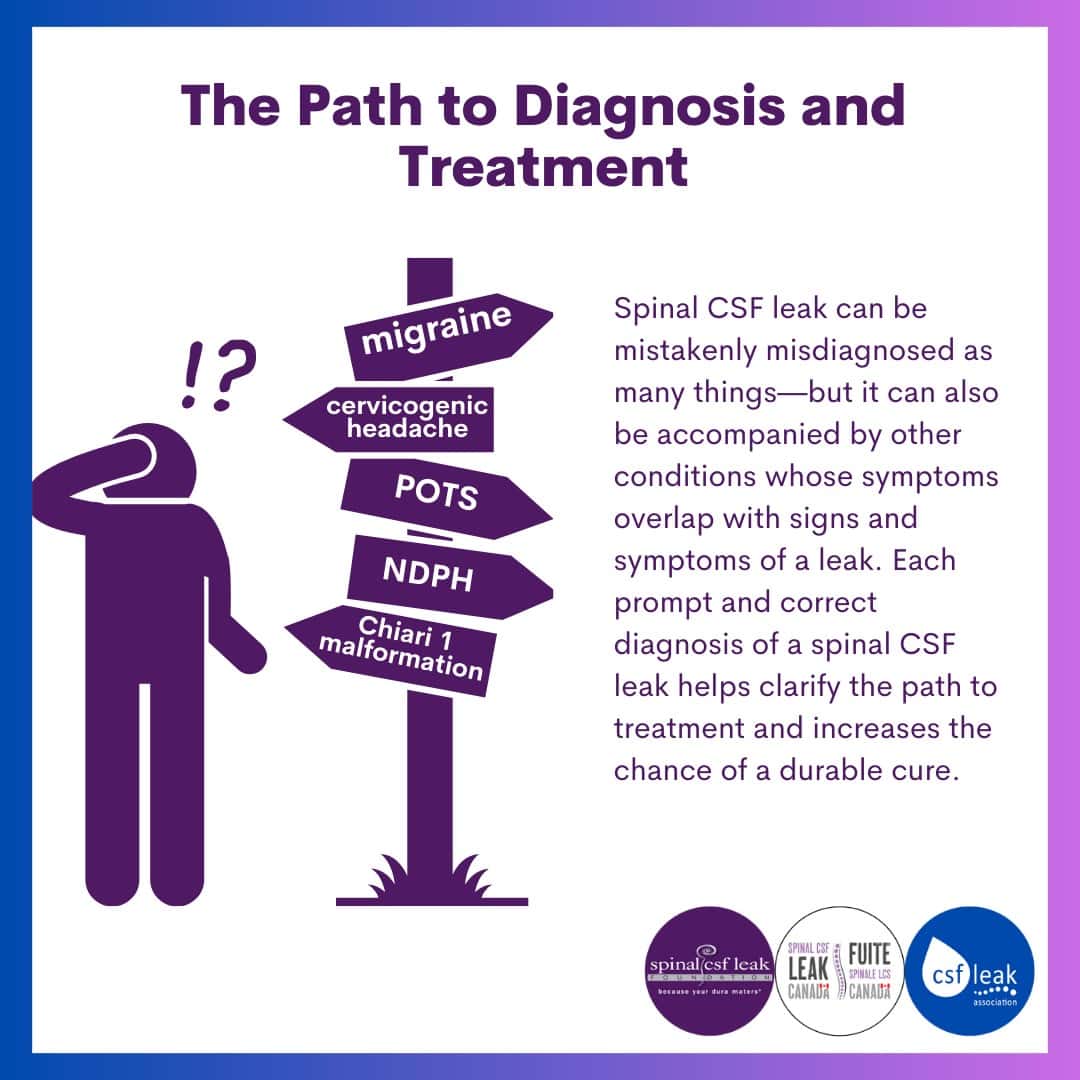
Some diagnoses that are often considered when evaluating for spinal CSF leak include: headache disorders, including migraine, tension headache, sinus headache, new daily persistent headache, and cervicogenic headache; occipital neuralgia or trigeminal neuralgia; meningitis; post-concussion syndrome; psychogenic disorder (arising from psychological issues); depression; anxiety disorders. Sometimes spinal CSF leak is misdiagnosed as one of these disorders, leading to a delay in proper treatment.
Diagnosing spinal CSF leak comes with many challenges. There is a wide variety of clinical presentation, and even the “hallmark” symptom of positional head pain is not seen in every patient. Not all head pain related to spinal CSF leak is position, and not every patient with positional head pain has a spinal CSF leak. Normal-appearing brain or spine imaging does not rule out the diagnosis. Additionally, interpretation of imaging requires experience and training, and can vary between specialists. And repeat imaging as well as more than one type of spinal imaging is often necessary.
Spinal CSF leak can be mistakenly misdiagnosed as many things—and can also be accompanied by other conditions whose symptoms overlap with signs and symptoms of a leak. Each prompt and correct diagnosis of a spinal CSF leak helps clarify the path to treatment and increases the chance of a durable cure.
Coming up tomorrow:
We discuss spinal CSF leak treatment.
Further information:
Spinal CSF Leak diagnosis main page (Spinal CSF Leak Foundation)