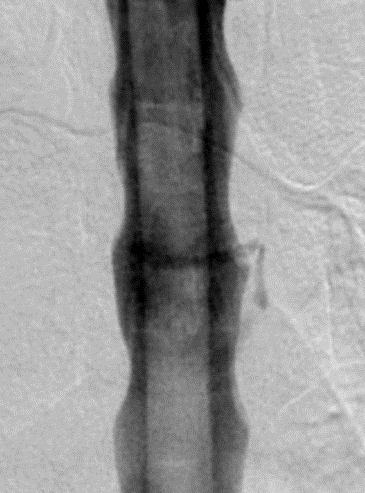
A variety of spinal imaging techniques are currently employed in patients with spontaneous intracranial hypotension to localize spinal CSF leaks. Digital subtraction myelography (DSM) is being used increasingly, most often to visualize the origin of rapid leaks.
A Digital Subtraction Myelogram = myelogram (injection of intrathecal contrast + imaging) is done under fluoroscopy with the ability to digitally subtract a pre-contrast image to enhance the view of the contrast. This is a dynamic form of imaging. This can be done under general anaesthesia to stop breathing for a short time, thereby preventing movement artifact on the imaging. A CT can be done soon after or with a bit of a delay.
Schievink et al have previously published on the use of this imaging technique, suggesting that in their experience, DSM is useful in identifying / localizing three types of spinal CSF leaks:
1) rapid leaks visible on MR or CT myelography as extensive longitudinal extradural fluid collections;
2) leaks ventral to the spinal cord;
3) CSF–venous fistulas between the subarachnoid space and spinal epidural veins that are not visualized on MR or CT myelography.
They have recently published again on this topic, specifically on their growing experience in the identification of spinal CSF-venous fistulas.
In this prospective study, 53 patients who met the ICHD-3 diagnostic criteria for spontaneous intracranial hypotension but without identifiable spinal CSF leak on recent spinal imaging, including conventional CT myelography, MRI or MR myelography, underwent DSM. Of these 53 patients, 42 had findings of intracranial hypotension on cranial MRI (in whom 9 had normalized); 10 had previous spinal imaging that had shown evidence of a spinal CSF, and 8 patients without cranial MRI or spinal imaging evidence of spinal CSF leak all had low opening pressure under 60 mm H20. DSM in 10 of the 53 patients revealed a CSF-venous fistula, all in the thoracic spine. Fistulas were found in those with and without previous abnormal cranial MRI findings and with and without previous spinal imagining evidence of CSF leak. The authors suggest that patients who meet the diagnostic criteria for spontaneous intracranial hypotension but in whom conventional spinal imaging fails to identify a spinal CSF leak, digital subtraction myelography should be considered.
Digital subtraction myelography for the identification of spontaneous spinal CSF-venous fistulas
Schievink WI, Moser FG, Maya MM, Prasad RS.
J Neurosurg Spine. 2016 Feb 5:1-5. [Epub ahead of print]
Abstract
OBJECTIVE In most patients with spontaneous intracranial hypotension, a spinal CSF leak can be found, but occasionally, no leak can be demonstrated despite extensive spinal imaging. Failure to localize a CSF leak limits treatment options. The authors recently reported the discovery of CSF-venous fistulas in patients with spontaneous intracranial hypotension and now report on the use of digital subtraction myelography in patients with spontaneous intracranial hypotension but no CSF leak identifiable on conventional spinal imaging (i.e., non-digital subtraction myelography).
METHODS The patient population consisted of 53 consecutive patients with spontaneous intracranial hypotension who underwent digital subtraction myelography but in whom no spinal CSF leak (i.e., presence of extradural CSF) was identifiable on conventional spinal imaging.
RESULTS The mean age of the 33 women and 20 men was 53.4 years (range 29-71 years). A CSF-venous fistula was demonstrated in 10 (19%) of the 53 patients. A CSF-venous fistula was found in 9 (27%) of the 33 women and in 1 (5%) of the 20 men (p = 0.0697). One patient was treated successfully with percutaneous injection of fibrin sealant. Nine patients underwent surgery for the fistula. Surgery resulted in complete resolution of symptoms in 8 patients (follow-up 7-25 months), and in 1 patient, symptoms recurred after 4 months.
CONCLUSIONS In this study, the authors found a CSF-venous fistula in approximately one-fifth of the patients with recalcitrant spontaneous intracranial hypotension but no CSF leak identifiable on conventional spinal imaging. The authors suggest that digital subtraction myelography be considered in this patient population.
PMID: 26849709
Other key references:
Headache secondary to intracranial hypotension.
Schievink WI, Deline CR.
Curr Pain Headache Rep. 2014 Nov;18(11):457.
Abstract
Intracranial hypotension is known to occur as a result of spinal cerebrospinal fluid (CSF) leaking, which may be iatrogenic, traumatic, or spontaneous. Headache is usually, but not always, orthostatic. Spontaneous cases are recognized more readily than in previous decades as a result of a greater awareness of clinical presentations and typical cranial magnetic resonance imaging findings. An underlying disorder of connective tissue that predisposes to weakness of the dura is implicated in spontaneous spinal CSF leaks. CT, MR, and digital subtraction myelography are the imaging modalities of choice to identify spinal CSF leakage. Spinal imaging protocols continue to evolve with improved diagnostic sensitivity. Epidural blood patching is the most common initial intervention for those seeking medical attention, and may be repeated several times. Surgery is reserved for cases that fail to respond or relapse after simpler measures. While the prognosis is generally good with intervention, serious complications do occur. More research is needed to better understand the genetics and pathophysiology of dural weakness as well as physiologic compensatory mechanisms, to continue to refine imaging modalities and treatment approaches, and to evaluate short- and long-term clinical outcomes.
PMID: 25255993
CSF-venous fistula in spontaneous intracranial hypotension: demonstration by digital subtraction myelography.
Schievink W, Moser F, Maya M.
Neurology. 2014 Jul;83:472-473
PMID: 24951475
Novel neuroimaging modalities in the evaluation of spontaneous cerebrospinal fluid leaks.
Schievink WI.
Curr Neurol Neurosci Rep. 2013 Jul;13(7):358.
doi: 10.1007/s11910-013-0358-z.
Abstract
Although for the vast majority of patients with spontaneous intracranial hypotension knowledge of the exact site of the underlying spinal CSF leak is not necessary, it is for patients with recalcitrant symptoms. Such patients may require directed treatments such as percutaneous fibrin glue injections or surgery. A variety of MRI techniques have been shown to be able to detect CSF leaks as well and sometimes better than the “gold standard” – CT-myelography. For unusually rapid CSF leaks – particularly those ventral to the spinal cord – digital subtraction myelography or dynamic CT-myelography are indicated. Some patients with spontaneous intracranial hypotension verified by intracranial MRI are never found to have a spinal CSF leak using current techniques.
PMID: 23703239
The role of digital subtraction myelography in the diagnosis and localization of spontaneous spinal CSF leaks.
Hoxworth JM, Trentman TL, Kotsenas AL, Thielen KR, Nelson KD, Dodick DW.
Am J Roentgenol. 2012 Sep;199(3):649-53.
doi: 10.2214/AJR.11.8238.
Abstract
OBJECTIVE:
The objective of our study was to review the clinical utility of digital subtraction myelography for the diagnosis of spinal CSF leaks in patients with spontaneous intracranial hypotension (SIH) and those with superficial siderosis.
MATERIALS AND METHODS:
Procedure logs from 2007 to 2011 were reviewed to identify cases in which digital subtraction myelography was performed to diagnose spinal CSF leaks. Electronic medical records were reviewed to obtain information regarding diagnosis and outcome. For patients to be included in the study, preprocedural spinal MRI had to show an extradural fluid collection spanning more than one vertebral level and postmyelographic CT had to confirm the presence of an active CSF leak. If digital subtraction myelography successfully showed the site of the CSF leak, the location was documented.
RESULTS:
Eleven patients (seven men and four women; mean age, 49.0 years) underwent digital subtraction myelography during the study period. Six patients had SIH and five patients had superficial siderosis. The extradural fluid collection on spinal MRI averaged a length of 15.5 vertebral levels. Digital subtraction myelography successfully showed the site of the CSF leak in nine of the 11 patients, and all of the dural tears were located in the thoracic spine between T3 and T11.
CONCLUSION:
Digital subtraction myelography is a valuable diagnostic tool for the localization of rapid spinal CSF leaks and should be considered in patients who are clinically suspected to have a dural tear that is accompanied by a
longitudinally extensive extradural fluid collection on spinal MRI.
PMID: 22915407