What is spontaneous intracranial hypotension?
Spontaneous intracranial hypotension from loss of CSF (cerebrospinal fluid) volume is the result of a defect in the spinal dura that allows leakage of CSF where it normally bathes and supports the brain and spinal cord. Seemingly spontaneous spinal CSF leaks may be related to underlying spinal pathology such as a calcified disc or bone spur, so in fact are not truly spontaneous.
Many spontaneous leaks appear to be related to an underlying structural weakness or thinning of the spinal dura, as evidenced by imaging and operative findings, as well as microscopic analysis of dural biopsies. Onset of symptoms, most often positional headache, occurs without clear precipitant or with relatively trivial mechanical factors in most of these cases.
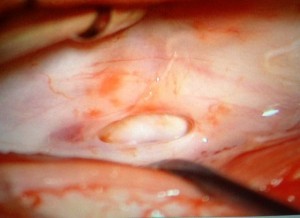
OR Image: defect in dura, shared with permission
How does this relate to Heritable Disorders of Connective Tissue (HDCT)?
Heritable disorders of connective tissue have been identified more frequently in people with spinal CSF leak than in the general population. Reported disorders include:
- Ehlers-Danlos Syndrome, classic type
- Ehlers-Danlos Syndrome, hypermobile type
- Marfan Syndrome
- Autosomal Dominant Polycystic Kidney Disease
- Aneurysms-Osteoarthritis Syndrome (Loeys-Dietz type 3)
Many additional patients have manifestations of Heritable Disorders of Connective Tissue (HDCT) that do not meet the diagnostic criteria for known disorders and might receive the diagnosis of unspecified HDCT. Symptoms and signs of intracranial hypotension may be the first clues that lead to a diagnosis of a HDCT.
Connective tissues are found throughout the body, so many organ systems can be affected in patients with HDCT. Dura is a connective tissue, just as skin, bones, muscles, joints and blood vessels are comprised of connective tissues.
Common findings of patients with HDCT
Here we list some of the more common findings, apart from abnormalities of dura, noted in personal medical history, family medical history, on clinical examination, or on imaging. These are listed by organ system.
Eyes:
- blue or gray sclera
- lens dislocation
- retinal detachment
- myopia
- early glaucoma
- early cataracts
Ears, Nose, Throat:
- high arched palate
- bifid uvula
- dental crowding
Musculoskeletal:
- tall stature
- slender habitus
- long limbs
- long fingers, toes
- scoliosis (curved spine)
- spondylolysis, spondylolisthesis (spine changes)
- Pectus deformities (chest sinks in or sticks out)
- joint hypermobility
- joint dislocations
- joint pain
- flat feet
Heart + blood vessels:
- bicuspid aortic valve
- mitral valve prolapse
- vertebral artery dissections
- carotid artery dissections
- aortic root dilatation (enlargement)
- aneurysms (intracranial, thoracic aorta, abdominal aorta, others)
- arterial tortuosity
Lungs:
- spontaneous pneumothorax (collapsed lung)
Skin:
- soft / thin / transparent skin
- stretchy skin
- easy bruising
- slow wound healing
- widened or thin scars
Brain / skull:
- congenital Chiari (note that intracranial hypotension may cause symptoms that appear to mimic Chiari 1 Malformation)
Spinal, muscle and joint abnormalities can result in much pain and disability. There may be impaired wound healing. More worrisome is that some cardiovascular manifestations have the potential for catastrophic outcomes. Thoracic aortic disease may result in rupture or dissections, both with high risk of mortality if not identified early. Aneurysms in other locations (brain, abdomen, pelvis) may also rupture. While additional study is needed to determine how often patients with spontaneous intracranial hypotension also have cardiovascular manifestations, preliminary evidence suggests that up to 20% have abnormalities on echocardiography and up to 9% have intracranial aneurysms.
In conclusion
It has been suggested that patients with spinal CSF leaks should be evaluated for other evidence of HDCT, which should include a detailed personal medical history, family medical history, and clinical examination, with attention to the items listed above. When an HDCT is suspected, clinical assessment might also include echocardiography to look for enlarged aortic root, aortic aneurysm or valvular abnormalities (more discussion that that here: Do I Need an Echo?). Additional screening for aneurysms and other vascular abnormalities might be considered on a case-by-case basis while we await more evidence to provide guidance. Some known heritable disorders of connective tissue are associated with a higher risk of vascular abnormalities while others are not. Decisions to do screening, for now, need to be individualized.
References:
Mokri B, Maher CO, Sencakova D. Spontaneous CSF leaks: underlying disorder of connective tissue.
Neurology. 2002 Mar 12;58(5):814-6.
Schrijver I, Schievink WI, Godfrey M, Meyer FB, Francke U. Spontaneous spinal cerebrospinal fluid leaks and minor skeletal features of Marfan syndrome: a microfibrillopathy. J Neurosurg. 2002 Mar;96(3):483-9.
Schievink WI, Gordon OK, Tourje J. Connective tissue disorders with spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension: a prospective study.
Neurosurgery. 2004 Jan;54(1):65-70; discussion 70-1.
Schievink WI. Spontaneous Spinal Cerebrospinal Fluid Leaks and Intracranial Hypotension. JAMA. 2006: 295(19):2286-2296.
Mokri B. Familial occurrence of spontaneous spinal CSF leaks: underlying connective tissue disorder. Headache. 2008 Jan;48(1):146-9.
Mokri B. Spontaneous CSF leaks: low CSF volume syndromes. Neurol Clin. 2014 May;32(2):397-422.
Schievink WI, Maya MM, Louy C, Moser FG, Sloninsky L. Spontaneous intracranial hypotension in childhood and adolescence. J Pediatr. 2013 Aug;163(2):504-10.
Reinstein E, Pariani M, Bannykh S, Rimoin DL, Schievink WI. Connective tissue spectrum abnormalities associated with spontaneous cerebrospinal fluid leaks: a prospective study. Eur J Hum Genet. 2013 Apr;21(4):386-90.
Liu FC, Fuh JL, Wang YF, Wang SJ. Connective tissue disorders in patients with spontaneous intracranial hypotension. Cephalalgia. 2011 Apr;31(6):691-5.
Albayram S, Baş A, Ozer H, Dikici S, Gulertan SY, Yuksel A. Spontaneous intracranial hypotension syndrome in a patient with marfan syndrome and autosomal dominant polycystic kidney disease. Headache. 2008 Apr;48(4):632-6.
Bassani L, Graffeo CS, Behrooz N, Tyagi V, Wilson T, Penaranda S, Zagzag D, Rifkin DB, Barcellos-Hoff MH, Fatterpekar G, Placantonakis D. Noninvasive diagnosis and management of spontaneous intracranial hypotension in patients with marfan syndrome: Case Report and Review of the Literature. Surg Neurol Int. 2014 Jan 21;5:8.
Koppen H, Baars MJ, van Gils A, Vis JC. Spontaneous Intracranial Hypotension as First Symptom of Aneurysms-Osteoarthritis Syndrome: A Case Report. Headache. 2015 Apr 15.
Schievink WI, Raissi SS. Spontaneous intracranial hypotension in patients with bicuspid aortic valve. J Heart Valve Dis. 2012 Nov;21(6):714-7.
Pimienta AL, Rimoin DL, Pariani M, Schievink WI, Reinstein E. Echocardiographic findings in patients with spontaneous CSF leak. J Neurol. 2014 Oct;261(10):1957-60.
Schievink WI, Maya MM. Frequency of intracranial aneurysms in patients with spontaneous intracranial hypotension. J Neurosurg. 2011 Jul;115(1):113-5.
