Spontaneous intracranial hypotension from spinal CSF leak is an important cause of headache, often quite disabling, that can be cured with treatment. The diagnosis, however, is not always as straightforward as one might imagine. Apart from low familiarity of an uncommon disorder, there are additional diagnostic challenges that physicians face.
Difficulty in distinguishing from other disorders
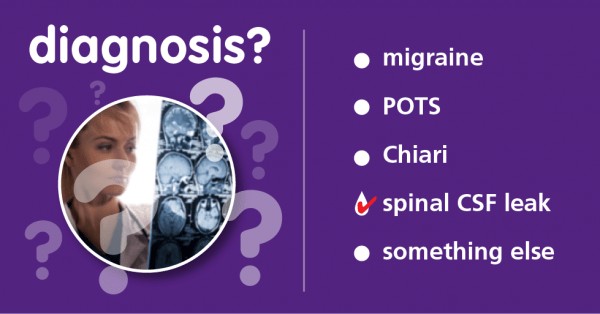
- One of the main diagnostic challenges is simply low awareness on the part of physicians. Patients may receive a diagnosis of common PRIMARY headache disorders, such as migraine headache or tension headaches, due to the lack of awareness of spinal CSF leak on the part of physicians. Greater awareness over the past decade has made this somewhat less common but there remains room for improvement.
- Headaches that are positional (orthostatic) tend to cause what is termed orthostatic intolerance, or difficulty tolerating upright posture. Not every patient with orthostatic intolerance has a spinal CSF leak. POTS, postural orthostatic tachycardia syndrome, is a type of autonomic nervous system dysfunction (dysautonomia) that causes a rise in heart rate and other changes after assuming upright posture, often with headache. Intracranial hypotension may be confused diagnostically with POTS and vice versa. To complicate matters further, intracranial hypotension and dysautonomia may both occur in the same patient at the same time.
- Not every headache related to a spinal CSF leak is positional. The headache may never have a positional component from onset. With chronicity, the positional aspect often lessens or even disappears. Occasionally, the positional aspect may be paradoxical, that is, worse when recumbent. The absence or lack of prominence of the positional aspect of the headache can make the diagnosis more challenging.
- The head pain is often located in the back of the head and can be confused with occipital neuralgia, which is pain arising from a nerve in that area.
- Headache may be mild or even absent with the result that the diagnosis may be less likely to be considered.
- Serious and atypical presentations such as dementia, tremor or Parkinsonism, ataxia or coma occur rarely, so intracranial hypotension as a potential underlying cause may not be entertained.
Confusion about intracranial pressure
- While low intracranial pressure is often seen, normal pressures do occur and do not rule out the diagnosis.
- Lumbar puncture to measure the opening pressure may be helpful but is not required to make the diagnosis.
Challenges with imaging
- CT of the head is often entirely normal, although subdural fluid collections may be noted. It is not the brain imaging of choice.
- Brain MRI with contrast is recommended in all cases in which the diagnosis is suspected. The mnemonic SEEPS summarizes the typical findings, yet normal imaging does occur and does not rule out the diagnosis. Recognition of findings does require experience or training.
- Subdural collections of fluid or blood are common on brain imaging and are not always recognized as the result of intracranial hypotension. This can lead to suboptimal treatment.
- A further diagnostic challenge is that descent of the brain from intracranial hypotension may be evidenced by low lying cerebellar tonsils on brain MRI and may be mistaken as congenital Chiari type 1 malformation. Intracranial hypotension may also result in worsening of a pre-existing congenital Chiari malformation.
- A range of spinal imaging (CT, MR, nuclear medicine) is used to evaluate and locate spinal CSF leaks but may not be straightforward to perform and/or interpret in all cases. For example, it may be difficult to find the precise source of a larger, faster leak such that specialized approaches may be required, such as dynamic CT myelography or digital subtraction myelography, not available in all centers. Smaller, slower leaks are not infrequently below the limits of sensitivity of currently available imaging techniques. There are additional circumstances that are best matched to specific imaging approaches. In many cases, patients will need to travel to centers seeing larger numbers of cases to access refined imaging techniques and expert interpretation.
Increasing Awareness
Fortunately, leaders in the field have been publishing new insights and findings which has increased awareness of this treatable secondary headache disorder.
Criteria have been published to help with the diagnostic challenges of SIH and spinal CSF leak: these are summarized HERE.
Educational efforts are assisting physicians in enhancing their understanding of clinical presentations, diagnostics, and treatments of intracranial hypotension secondary to spinal CSF leak.
