A new publication features the remarkable case of a spinal CSF leak whose cause turned out to be a labor epidural from almost 18 years earlier—that’s right, 18 years.
Drs. Callan. Lennarson, and Carroll report on this fascinating story in their paper, “A causative role for remote dural puncture and resultant arachnoid bleb in new daily persistent headache: A case report,” just published in the journal Headache.
During labor roughly 18 years ago, this patient was given epidural anesthesia. Afterwards, she experienced what’s called a “post-dural puncture headache”—head pain that occurs after the dura mater has been punctured during a medical procedure, causing intracranial hypotension. But after 24 hours of bedrest, the headache went away, and all seemed well.
Twelve years later, she began exhibiting symptoms of a spinal CSF leak. Since these symptoms developed so long after her labor epidural experience, it wasn’t even suggested that they could be due to a spinal CSF leak caused by that long-ago dural puncture. And with no apparent imaging findings on MRI or CT, she was given the diagnosis of “new daily persistent headache.”
For nearly six years, she was bedridden while she fought to obtain the proper diagnosis and treatment.
Finally, the cause of her spinal CSF leak was discovered: a tiny arachnoid bleb right where that original epidural anesthesia had been administered, nearly 18 years before.
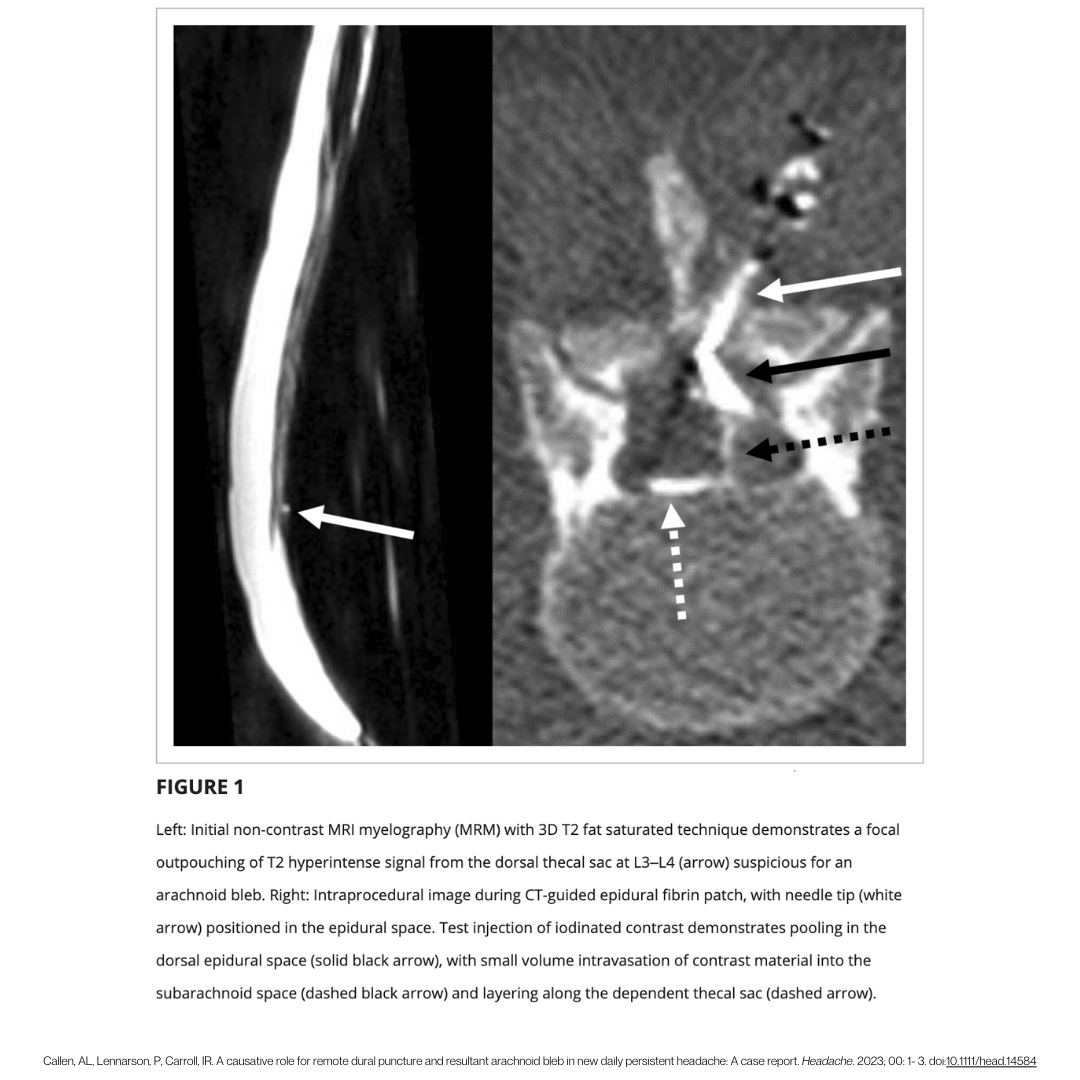
It’s important to note that this bleb was able to be seen on the initial non-contrast MRI the patient originally had done when her symptoms first began, but at the time it wasn’t recognized as a possible source of her symptoms. Six years later, the bleb was addressed via surgery,

Further reading:
, , . A causative role for remote dural puncture and resultant arachnoid bleb in new daily persistent headache: A case report. Headache. 2023; 00: 1– 3. doi:10.1111/head.14584