CT-fluoroscopy-Guided Ventral CSF Leak Patching
Shared with permission from Timothy Amhrein, MD and Duke University Medical Center
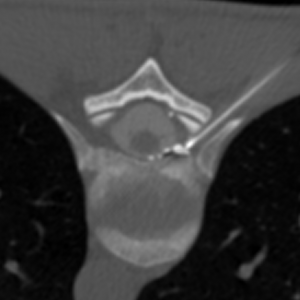
Several centers in the USA and elsewhere that see larger numbers of patients with spinal CSF (cerebrospinal fluid) leaks are continually refining their approaches in diagnosis and treatment. The team of neuroradiologists at Duke University Medical Center that perform spine procedures for patients has published a new paper describing refinements in technique for a subset of spinal CSF leaks. This subset, ventral CSF leaks (those that occur in front of the spinal cord), has been more challenging to treat with percutaneous (injection) techniques rather than open surgery. They used CT-fluoroscopy guidance for precise needle placement with a specific approach and found the procedure to be safe with an excellent technical success rate.
CT Fluoroscopy-Guided Blood Patching of Ventral CSF Leaks by Direct Needle Placement in the Ventral Epidural Space Using a Transforaminal Approach.
Amrhein TJ, Befera NT, Gray L, Kranz PG.
AJNR Am J Neuroradiol. 2016 Jul 7. [Epub ahead of print]
Author information
Abstract
BACKGROUND AND PURPOSE:
Epidural blood patch treatment of spontaneous intracranial hypotension arising from ventral CSF leaks can be difficult secondary to challenges in achieving ventral spread of patching material. The purpose of this study was to determine the technical success rates and safety profile of direct needle placement into the ventral epidural space via a posterior transforaminal approach.
MATERIALS AND METHODS:
We retrospectively reviewed consecutive CT fluoroscopy-guided epidural blood patches from June 2013 through July 2015. Cases were included if a posterior transforaminal approach was taken to place the needle directly in the ventral epidural space. Rates of technical success (defined as contrast in the spinal canal ventral epidural space) and optimal epidurogram (defined as contrast spreading into or beyond the middle third of the spinal canal ventral epidural space) were determined. Factors influencing these rates were assessed. All complications, inadvertent intravascular injections, and intrathecal punctures were recorded.
RESULTS:
A total of 72 ventral epidural blood patches were identified; immediate technical success was achieved in 95.8% and an optimal epidurogram in 47.2%. Needle position within the spinal canal ventral epidural space was associated with obtaining an optimal epidurogram (P = .005). Inadvertent intravascular injection was identified in 29.3% of cases, but all were venous. There were no inadvertent intrathecal punctures or complications.
CONCLUSIONS:
Direct needle placement in the ventral epidural space via a transforaminal approach for treatment of ventral CSF leaks has an excellent technical success rate and safety profile. This technique can be considered as a treatment option in selected patients with ventral CSF leaks for whom traditional techniques are unsuccessful.
© 2016 American Society of Neuroradiology.
PMID: 27390315
DOI: 10.3174/ajnr.A4842

